- 99% BOREDOM - 20 Jan 2026
- THE ENDOTRACHEAL TUBE IS YOUR FRIEND - 7 Jan 2026
- ANESTHESIOLOGIST NAMES ON OUR HATS = A SOLID IDEA - 16 Dec 2025

Emma Stone in Poor Things
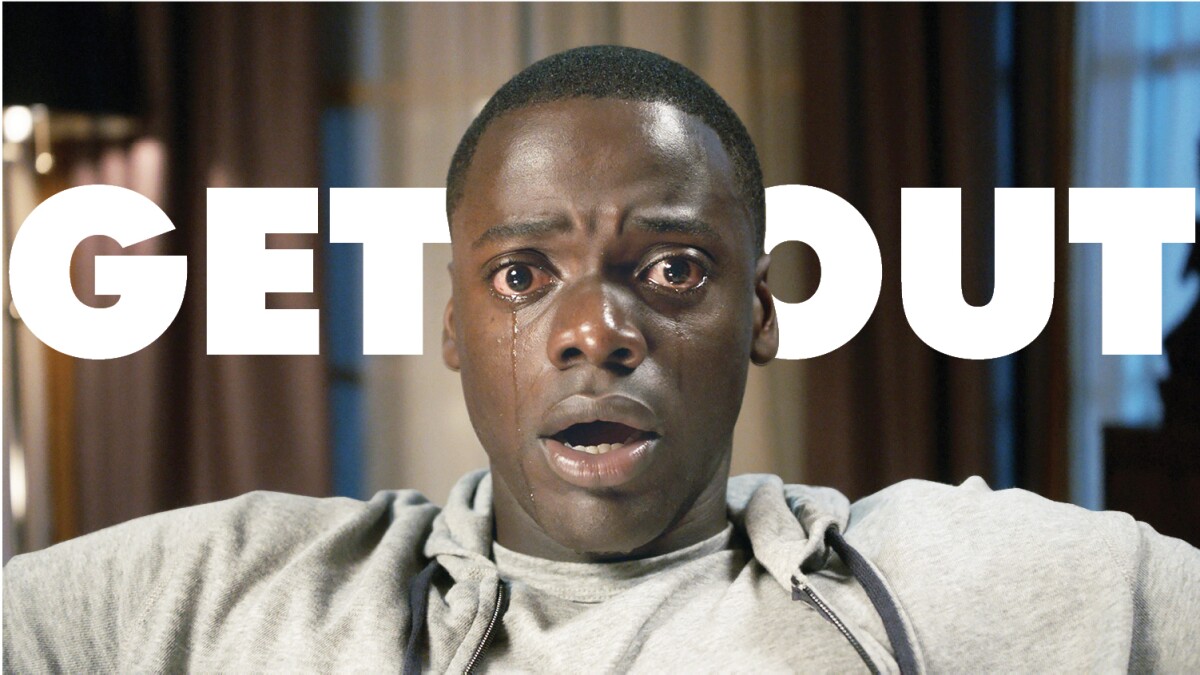
Daniel Kaluuya in Get Out
The movie Poor Things was nominated for the 2024 Academy Award for Best Picture. Poor Things starlet Emma Stone won the Best Actress Oscar for her role as a woman who received a brain transplant from an infant. The plot of the movie was impossible without the notion of brain transplantation, which was performed in the surgeon’s home. The 2017 Jordan Peele movie Get Out earned $255 million with its premise that a neurosurgeon was transplanting the brains of wealthy elderly humans into the bodies of young healthy Black men. Again the plot of the movie was impossible without the notion of brain transplantation. How feasible is brain transplantation? Every transplantation requires an anesthesiologist, and I’m qualified to answer this question for you.
An Italian neurosurgeon named Sergio Canavero believes brain transplantation is technically feasible. In 2020 he published a book entitled THE TECHNOLOGY OF BRAIN TRANSPLANTATION. The book is available on Amazon. In 2022 he published an article in Surgery Neurology International entitled “Whole Brain Transplantation in Man: Technically Feasible.” The article discussed BRAVE, the BRain Anastomosis Venture, which is part of a larger project which aims at transplanting a brain into a young immune-conditioned body. Canaveros explains that the concept of a brain transplant, also known as a cerebro-somatic anastomosis, is currently thought to be “unachievable.” He lists the following roadblocks to successful brain transplantation:
- “Impossibility to extract the brain proper from the dura mater.” Removing the skull bones covering the brain is a straightforward task for neurosurgeons. The exposed brain is encased in the three thin layers of the meninges: the dura, the arachnoid, and the pia, which line the entire brain and spinal cord. Separating the dura from the brain is thought to be impossible. Canaveros describes his proposed technique in which the surrounding meninges and dura are transplanted along with the brain. The brain, encased in the dura, is freed from the cranial vault and base, and a robotic scoop with retractable tines would be brought into the operating field. The scoop envelops the brain and supports it as the dural detachment proceeds, and facilitates the final transfer into the new skull base. [See Figure 2 below)

- “Impossibility to resuture the internal carotid and vertebral arteries and the internal jugular veins once the brain is laid on the donor’s skull base.” Brain transplantation requires a rapid restart of blood circulation into the implanted brain as soon as possible. Brain cells are known to die within five minutes if deprived of oxygen. Once the new brain is inserted into the skull base, there is no longer any room to utilize needles and suture to sew the arteries and veins back together. Canaveros describes alternative means of reconnecting vascular structures without sutures. Options for sutureless vascular anastomosis [anastomosis = a medical word for the connection between two adjacent tubes or channels] include: a) an expandable stent inserted in both stumps, in which the stumps are then approximated, the stent is fully expanded, and an adhesive adds stability to the coaptation [this is called stent-assisted vascular anastomosis]; b) a polymer can be injected into the lumen of the vessels, and an adhesive stabilizes the complex while the polymer solidifies; c) a nonresorbable stent with pins, which once deployed, can close the anastomosis; or d) magnetic connectors inserted into the two stumps which can ensure immediate coaptation, called Magnetic Anastomosis.(See Figure 3 below)

- “Lack of an efficient technology to functionally reconnect the 12 pairs of cranial nerves.” Twelve cranial nerves exit the brain on both the right and left sides. These nerves supply motor and sensory innervation to the head and neck, including the senses of sight, hearing, balance, smell, and taste. Brain transplantation would only be acceptable if rapid recovery of neural transmission ensues. The patient is expected to emerge from post-transplant-induced anesthesia with cranial nerve function already present or rapidly recovering. Similarly to vascular reconnection in 2. above, the traditional reconnection of severed nerves with suture is not feasible. Besides the constrained operative space, microsuturing cannot reestablish cranial nerve function rapidly, and therefore regeneration cannot be expected to occur rapidly. Cranial nerves carry complex information to the brain. Each cranial nerve has approximately 100,000 axons, and the optic nerve has approximately 1,200,000 fibers. Suturing would traumatize the nerve. Canaveros describes techniques of neural fusion and sutureless nerve anastomosis, which aim to solve this problem.
- “Lack of a technology to reconnect the severed spinal cord.” The implanted brain needs to be quickly connected to the spinal cord, which carries neural impulses to and from the rest of the body. Once sharply severed, the spinal cord has been functionally reconnected in a primate model (see the GEMINI protocol: Fully reviewed in Canavero and Ren), but this has never been done in humans.
- “Undetermined neuroprotective measures to deploy between the moment of physical separation of the brain from [the old] skull and re-establishment of circulation after positioning on [the new] skull base.” Profound hypothermia can protect the brain by lowering the metabolic rate of the brain and therefore lowering oxygen demand. Applying some form of this technology to the transplanted brain would likely be necessary to preserve the function of its neurons during the transfer. Brain protection through profound hypothermia was demonstrated 50 years ago in primates and more recently confirmed in China.
- “Possible immune rejection if brain transplantation is carried out on a heterologous body rather than [the brain’s] clone.” The blood-brain barrier protects the brain from the white blood cells and antibody attacks of the immune response. A transplanted brain may have a breakdown of this barrier, making it vulnerable to rejection. Canaveros postulates that brain transplantation into a clone of the transplanted brain might not require immunosuppressants. He also describes that protocols are being developed that may be used for heterologous (non-clone) brain transfers.
A massive deal of research in animals would be needed to solve these six problems prior to any possible human brain transplantation.
ANESTHETIC CONSIDERATIONS FOR BRAIN TRANSPLANTATION:
There are no published data to refer to regarding anesthesia for brain transplantation. The primary anesthetic issues for brain transplantation would be:
- How to keep brain cells alive during the transplant procedure? Brain cells are extremely sensitive to lack of oxygen and lack of blood flow. Brain cells are known to die within 5 minutes without oxygen. Because transplantation requires severing the donor blood supply to the brain, how can brain cell life be preserved during the transfer to the recipient body? Current medical technology has no answer to this problem. I’m not aware of any action (e.g. cooling the cells or pharmacologically decreasing the metabolic rate of the cells) which would maintain brain cell viability in the absence of normal blood flow, and under the best of circumstances, it would take multiple minutes to reattach blood flow to the brain. This issue is the primary medical challenge to brain transplantation.
- What sort of operating room setup would be required for brain transplantation? Could brain transplantation ever occur in a neurosurgeon’s basement, as in Get Out or Poor Things? No. The transplant would require two fully-staffed neurosurgical operating rooms. The donor and recipient bodies would need to be anesthetized by two separate teams of anesthesiologists in these adjacent rooms, to minimize the time the oxygen-deprived brain was not perfused with blood during the transfer. High-tech medical equipment would need to be immediately available, and professionals trained to deploy such devices would need to be present. The entire undertaking would require the resources of a major medical center, not a stripped down version of an operating room table in someone’s house.
- The recipient body with its new brain would need postoperative intensive care unit (ICU) care for several days. Again this is level of technology not available in someone’s basement.
ANESTHETIC TECHNIQUE. Again, there are no published data to refer to regarding anesthesia for brain transplantation. What follows are speculations based on fundamentals of neuroanesthesia:
THE DONOR:
The brain donor body would require an anesthetic team to monitor vital signs and to maintain these vital signs as normal as possible prior to disconnecting the brain.
- The donor would be positioned supine. In addition to standard anesthesia vital signs monitors, the donor would require an arterial line and a central venous pressure line equipped with vasoactive drips to maintain blood pressure within normal limits.
- Vital sign values would guide the anesthesiologist in his/her goals to maintain cerebral blood flow, cerebral perfusion pressure, mean arterial pressure, and intracranial pressure within normal limits, to preserve normal brain function.
THE RECIPIENT:
The brain recipient body would require an anesthetic team to monitor the vital signs and to keep the vital signs as normal as possible prior to receiving the new brain.
- The donor would be positioned supine. In addition to standard anesthesia vital signs monitors, the donor would require an arterial line and a central venous pressure line equipped with vasoactive drips to maintain blood pressure within normal limits.
- Vital sign values would guide the anesthesiologist in his/her goals to maintain cerebral blood flow, cerebral perfusion pressure, mean arterial pressure, and intracranial pressure within normal limits, to preserve normal brain function. The anesthesiologist would avoid hypertension, hypotension, tachycardia, and bradycardia.
- There is no data on the preferred general anesthetic drug recipe or technique, but a combination of remifentanil/propofol/sevoflurane is a likely choice. The physicians would minimize the time from when one brain came out and the new brain was transplanted. The anesthesiologists would keep the mean arterial pressure at low normal values while the vascular anastomoses were being done, to minimize blood loss. The anesthesiologists would likely employ minimal hyperventilation as needed to decrease end-tidal CO2 and evoke brain shrinkage for better surgical exposure.
- The patient would be transferred to the ICU postoperatively. The patient would be sedated with intravenous propofol and/or dexmedetomidine until it was clear that all vascular anastomoses were intact. The patient could then be awakened for neurologic checks.
- Vital signs, including oxygenation, would be kept normal as possible throughout the postoperative course.
Would brain transplantation be ethical, even if it were possible? Consider that a brain transplant is really a body transplant—the donation of an entire new body to a someone else’s brain. Will it ever make sense to use a full donor body to save one life? Or should that donor’s organs go to multiple individuals, potentially saving many lives?
Wikipedia lists 26 movies under the heading of “Films about brain transplantation.”

Similar to time-travel movies (e.g. Back to the Future or Outlanders), and faster-than-light-speed interstellar movies (e.g. Star Wars or Star Trek), stories about human brain transplantation must be considered science fiction—that is, they are entertaining tales which the educated viewer must perceive as quite impossible.
*
*
The most popular posts for laypeople on The Anesthesia Consultant include: How Long Will It Take To Wake Up From General Anesthesia? Why Did Take Me So Long To Wake From General Anesthesia? Will I Have a Breathing Tube During Anesthesia?What Are the Common Anesthesia Medications? How Safe is Anesthesia in the 21st Century? Will I Be Nauseated After General Anesthesia? What Are the Anesthesia Risks For Children?
The most popular posts for anesthesia professionals on The Anesthesia Consultant include: 10 Trends for the Future of Anesthesia Should You Cancel Anesthesia for a Potassium Level of 3.6? 12 Important Things to Know as You Near the End of Your Anesthesia Training Should You Cancel Surgery For a Blood Pressure = 170/99?Advice For Passing the Anesthesia Oral Board Exams What Personal Characteristics are Necessary to Become a Successful Anesthesiologist?
READ ABOUT RICK NOVAK’S FICTION WRITING AT RICK NOVAK.COM

