emailrjnov@yahoo.com
- BRAIN TRANSPLANTATION? - 28 Mar 2024
- THE ANESTHESIA CONSULTANT NAMED THE #1 ANESTHESIOLOGY BLOG IN THE WORLD FOR 2024 BY FEEDSPOT - 7 Mar 2024
- AN ANESTHESIA STORY LIKE NO OTHER - 2 Mar 2024
A 12-year-old boy and his mother walk into a surgery center. The child is scheduled for a tonsillectomy, and is otherwise healthy. The anesthesiologist induces general anesthesia, and ten minutes later the patient has ventricular arrhythmias which descend into a cardiac arrest. Advanced Cardiac Life Support (ACLS) measures are applied, but the child cannot be resuscitated, and is declared dead. What caused this cardiac arrest during a pediatric tonsillectomy?
This is an actual closed malpractice case which I was asked to review. The anesthesiologist induced general anesthesia with propofol and a paralytic drug called succinylcholine (sux-in-ol-KOH-leen), and then inserted a breathing tube successfully into the patient’s windpipe. All vital signs were normal. Sevoflurane, nitrous oxide, and 50% oxygen were ventilated into the patient’s lungs. The surgeon began the tonsillectomy. One minute later the cardiac arrest occurred. The anesthesiologist followed ACLS guidelines, but standard ACLS treatments and hyperkalemia (elevated potassium concentration) treatments were unsuccessful.

Succinylcholine is an intravenous muscle relaxant (paralytic) drug commonly used in the United States. Succinylcholine is an old drug—available since 1951—which has the distinction of being the most rapid-acting intravenous muscle relaxant, and also the shortest-acting muscle relaxant. Succinylcholine is an important drug in an anesthesiologist’s toolkit. When an airway emergency threatens a patient’s life, such as the unexpected occurrence of laryngospasm, succinylcholine is the emergency drug of choice to paralyze the patient, relax the spasm of the vocal cords, and enable the anesthesiologist/emergency room physician/acute care physician to insert a life-saving breathing tube into the trachea.
But succinylcholine can be a dangerous drug. The Food and Drug Administration (FDA) placed a Black Box Warning on succinylcholine in 1994. The current succinylcholine warning in the PDR (Prescribers’ Digital Reference) reads:
“Succinylcholine is contraindicated in patients with a personal or familial history of malignant hyperthermia and/or skeletal muscle myopathy. Malignant hyperthermia may be precipitated by succinylcholine; concomitant use of volatile anesthetics may further increase this risk.
In neonates, infants, children, and adolescents, reserve the use of succinylcholine for emergency intubation or instances where immediate securing of the airway is necessary (e.g., laryngospasm, difficult airway, full stomach, or lack of intravenous access).
There have been rare reports of ventricular dysrhythmias and fatal cardiac arrest secondary to rhabdomyolysis with hyperkalemia, primarily in healthy-appearing pediatric patients who were subsequently found to have undiagnosed skeletal muscle myopathy, most frequently Duchenne’s muscular dystrophy.
Affected pediatric patients are typically, but not exclusively, males 8 years or younger. Although some patients have no identifiable risk factors, a careful history and physical exam may identify developmental delays suggestive of myopathy, and a preoperative creatinine kinase could identify patients at risk.
Closely monitor body temperature, expired CO2, heart rate, blood pressure, and electrocardiogram in pediatric patients to help detect early signs of malignant hyperthermia and/or hyperkalemia.
The rhabdomyolysis syndrome often presents as peaked T-waves and sudden cardiac arrest within minutes of succinylcholine administration. If cardiac arrest occurs immediately after succinylcholine administration, institute treatment for hyperkalemia (e.g., intravenous calcium, bicarbonate, glucose with insulin, hyperventilation). If malignant hyperthermia is suspected, initiate appropriate treatment (e.g., dantrolene, supportive care) concurrently.”
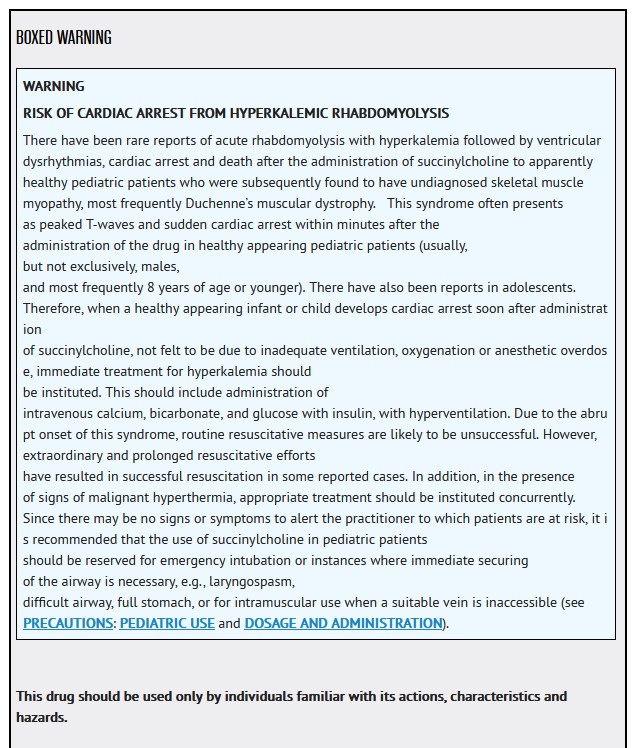
Per the Black Box warning, succinylcholine has the potential for inducing life threatening hyperkalemia in children with undiagnosed skeletal muscular dystrophies. Severe hyperkalemia and ventricular arrhythmias followed by cardiac arrest may occur in apparently healthy children who have an occult muscular dystrophy (usually Duchenne’s muscular dystrophy). An occult muscular dystrophy is a rare inherited disease. The global prevalence of Duchenne’s muscular dystrophy is 7.1 cases per 100,000 males, and 2.8 cases per 100,000 in the general population. The Black Box warning on succinylcholine recommends to “reserve use in children for emergency intubation or need to immediately secure the airway.”
The Black Box warning applies to neonates, infants, children and adolescents. No parent wants their son or daughter under the age of 18 to electively receive a drug which has an FDA Black Box Warning for use in adolescents. No parent wants their neonate, infant, child, or adolescent to have a risk of sudden cardiac arrest under general anesthesia for a common elective surgery.
In 1994 the Anesthesia Patient Safety Foundation (APSF) published a sentinel article about the risks of succinylcholine in pediatric anesthesia. The article reviews the history of the succinylcholine warning: “In 1992, Drs. H. Rosenberg and G. Gronert published a letter in Anesthesiology briefly reviewing four deaths in male children under the age of eight who had received halothane and then succinylcholine. These cases were identified through the Malignant Hyperthermia (MH) Hotline. Reference was also made to ‘11 similar cases’ identified through the German MH Hotline. Their letter concluded with the statement: ‘We have notified the Food and Drug Administration of this potential problem and recommended that anesthesiologists carefully consider the indications for use of succinylcholine in young children.’ This letter was accepted for publication August 24,1992.” The article goes on to emphasize “the need for prompt and appropriate treatment should hyperkalemic arrest occur. This treatment involves the intravenous administration of calcium. With proper treatment, approximately 50% of patients have survived this catastrophic hyperkalemia.” The Black Box warning specifically states, “If cardiac arrest occurs immediately after succinylcholine administration, institute treatment for hyperkalemia (e.g., intravenous calcium, bicarbonate, glucose with insulin, hyperventilation).”
Despite the Black Box warning, how often is succinylcholine still used for non-emergency pediatric anesthetics in the United States? No one knows. I can attest that during a recent Quality Assurance review in the Northern California, I saw anesthetic records from a board-certified anesthesiologist who administered succinylcholine to a 14-year-old boy for elective ear surgery. I discussed this with the anesthesiologist, who was unaware they were doing anything dangerous.
There is an excellent alternative to the elective use of succinylcholine. For most cases, pediatric or adult, the muscle relaxant rocuronium is a superior alternative to succinylcholine. Succinylcholine is the IV muscle relaxant with the most rapid onset, but large doses (0.9 mg/kg) of rocuronium are nearly as rapid as succinylcholine, without any of succinylcholine’s risks. Succinylcholine is also the IV muscle relaxant which wears off the fastest, but since the year 2015 FDA approval of the muscle relaxant reversal drug sugammadex (Bridion), an intubating dose of rocuronium can be rapidly reversed within 3 minutes by administering 16 mg/kg of sugammadex.
Succinylcholine remains an important drug for the treatment of airway emergencies. I would never begin a general anesthetic if I did not have a vial of succinylcholine immediately available in case of an airway emergency. In addition, succinylcholine is important because it can be administered intramuscularly (in a patient who has no IV). For example, if a child is undergoing an inhalational induction of general anesthesia with sevoflurane vapor prior to a surgery, and the child suddenly goes into laryngospasm before any IV can be started, (this does occur, not uncommonly, and is a true emergency), the appropriate treatment is an intramuscular injection of 4 mg/kg of succinylcholine. The child will become paralyzed within minutes, and the anesthesiologist can then insert a life-saving breathing tube. (The mean onset of paralysis with 4 mg/kg intramuscular succinylcholine in children ages 1 to 10 ranges from 2.9 to 3.9 minutes.)
I’ve written about the advantages and risks of succinylcholine previously in the article, “Succinylcholine: Vital Drug or Obsolete Dinosaur?”
I also refer you to the published article, “Is There Still a Role for Succinylcholine in Contemporary Clinical Practice?“
The take home messages from this case study of a cardiac arrest during a pediatric tonsillectomy are:
- If you’re an anesthesia provider, do not administer succinylcholine to a neonate, infant, child, or adolescent for an elective surgery. The Black Box warning on succinylcholine recommends to “reserve use in children for emergency intubation or need to immediately secure the airway.”
- If you’re a parent, prior to your son or daughter’s surgery, be empowered to ask your child’s anesthesiologist if they’re aware of the Black Box warning on succinylcholine.
- Nobody wants a death brought on by an elective anesthetic.

*
*
*
The most popular posts for laypeople on The Anesthesia Consultant include:
How Long Will It Take To Wake Up From General Anesthesia?
Why Did Take Me So Long To Wake From General Anesthesia?
Will I Have a Breathing Tube During Anesthesia?
What Are the Common Anesthesia Medications?
How Safe is Anesthesia in the 21st Century?
Will I Be Nauseated After General Anesthesia?
What Are the Anesthesia Risks For Children?
The most popular posts for anesthesia professionals on The Anesthesia Consultant include:
10 Trends for the Future of Anesthesia
Should You Cancel Anesthesia for a Potassium Level of 3.6?
12 Important Things to Know as You Near the End of Your Anesthesia Training
Should You Cancel Surgery For a Blood Pressure = 170/99?
Advice For Passing the Anesthesia Oral Board Exams
What Personal Characteristics are Necessary to Become a Successful Anesthesiologist?
READ ABOUT RICK NOVAK’S FICTION WRITING AT RICK NOVAK.COM.

