emailrjnov@yahoo.com
- THE TOP 10 SURGICAL ADVANCES OF THE LAST 70 YEARS - 30 Apr 2024
- BRAIN TRANSPLANTATION? - 28 Mar 2024
- THE ANESTHESIA CONSULTANT NAMED THE #1 ANESTHESIOLOGY BLOG IN THE WORLD FOR 2024 BY FEEDSPOT - 7 Mar 2024
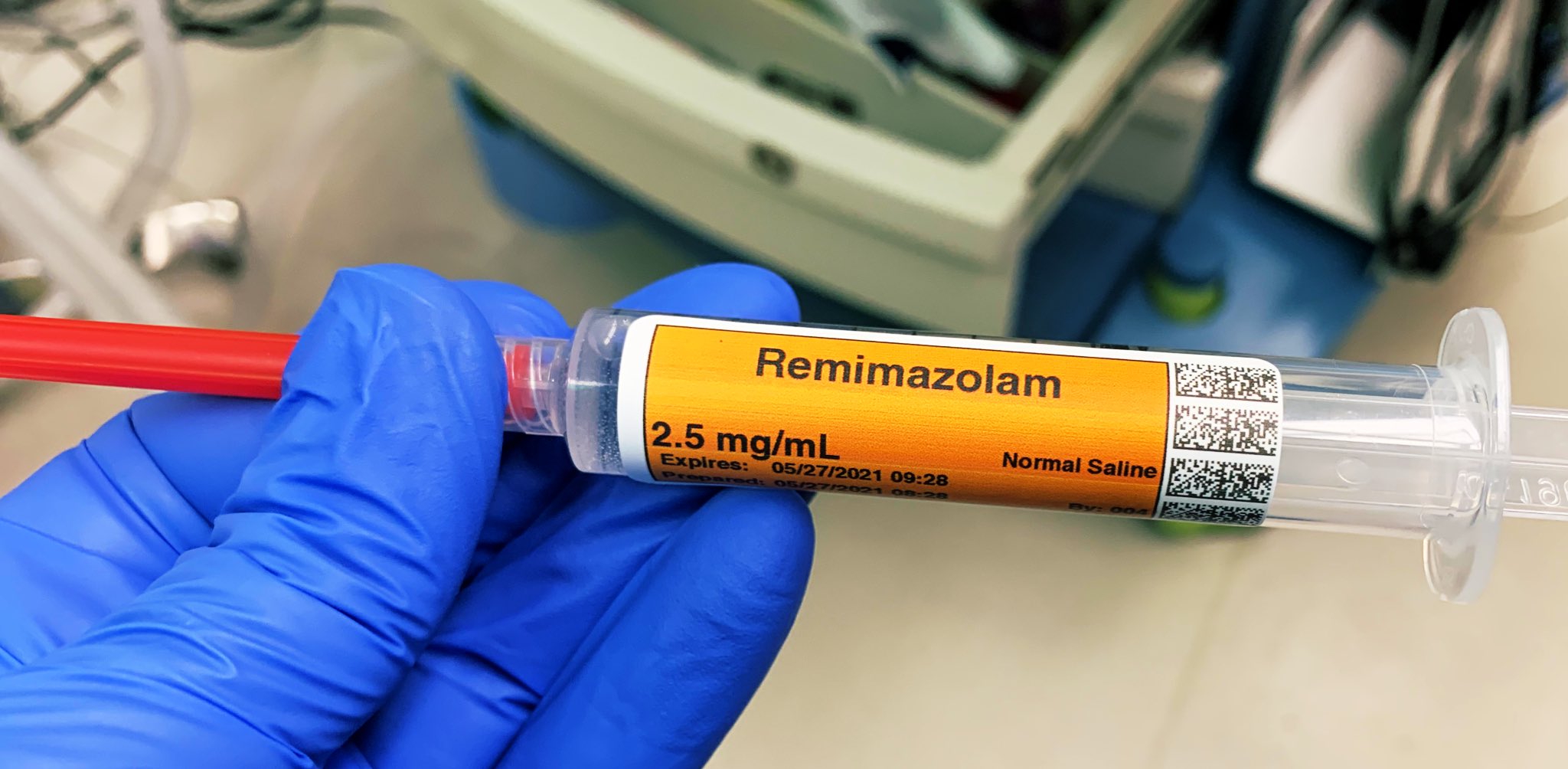
In July 2020 the Food and Drug Administration (FDA) approved the intravenous benzodiazepine remimazolam (Byfavo, Acacia Pharma) for use in sedation for procedures of 30 minutes or less. Will anyone utilize this new drug, or is it an expensive addition to our arsenal with few significant advantages over current agents?

Remimazolam differs from midazolam (Versed), the current most commonly used IV benzodiazepine, in that remimazolam is rapidly converted to an inactive metabolite by tissue esterases, resulting in an ultra-short onset/offset profile. Remimazolam is marketed as a powder which must be reconstituted into a liquid within its vial prior to administration.

For use in procedural sedation, remimazolam will not replace Versed, but rather will aim to replace propofol. The proposed advantages of remimazolam over propofol include:
- Remimazolam can be completely reversed by the benzodiazepine antagonist flumazenil (Romazicon) whereas there is no reversal agent or antagonist for propofol. The only way to end the sedative effects of propofol is for an anesthesia professional to support the airway, breathing, and circulation of the patient until the drug effects of propofol wear off in time.
- Remimazolam has minimal cardiac or respiratory depression. Sicker ASA III and IV patients maintain their breathing and circulation status while under remimazolam sedation.
- There is no accumulative effect of remimazolam over time. Its elimination by an esterase does not slow during lengthy administration of remimazolam, as in the prolonged sedation of an intensive care unit (ICU) patient on a ventilator.
- There is no burning sensation upon injecting remimazolam into a patient’s intravenous line as there is with propofol.
- A non-anesthesia-professional can administer remimazolam, whereas an anesthesia professional/airway expert must administer and monitor propofol administration.
Are these advantages important? Items 1 – 5 are discussed as follows:
- Non-anesthesiologists can reverse the effects of remimazolam with flumazenil if they overdose a patient, but this advantage is less important for anesthesia professionals. Anesthesiologists can manage the airway of a patient over-sedated with a benzodiazepine without need to administer a reversal agent. I’ve never administered a dose of flumazenil in my entire career, nor have most of my anesthesia colleagues.
- Propofol has cardiac and respiratory depression, but in most cases these effects are minimal. Per the PDR (Physician’s Digital Reference), patients with compromised myocardial function, intravascular volume depletion, or abnormally low vascular tone (e.g. septic patients) are more susceptible to hypotension. When an anesthesiologist is present these risks are routinely managed.
- For a long operating room anesthesia case (e.g. of 8 – 10 hours duration), there is no clinically significant accumulation of propofol in the bloodstream. Propofol Infusion Syndrome (PRIS), which can be potentially fatal, is a risk with prolonged propofol sedation in the ICU (See ICU Sedation below).
- The burning sensation upon injecting propofol can be blunted by intravenous lidocaine. A 2016 meta-analysis showed that both lidocaine pretreatment and mixing lidocaine with the propofol were effective in reducing pain on propofol injection. In addition, a preanesthetic dose of Versed prevents a patient from remembering any burning sensation from a propofol injection that follows.
- The most important advantage of remimazolam is that non-anesthesiologists can safely administer remimazolam. Propofol administration requires an experienced clinician, e.g. either an anesthesiologist, a certified registered nurse anesthetist (CRNA), or an emergency medicine physician. Per the American Society of Anesthesiologists: “The practitioner administering propofol for sedation/anesthesia should, at a minimum, have the education and training to identify and manage the airway and cardiovascular changes which occur in a patient who enters a state of general anesthesia.”
The disadvantages of remimazolam compared to propofol include:
- Expense. The cost of a 20 ml (200 mg) vial of propofol is $9.20. The cost of a 20 mg vial of powdered remimazolam is $41.67.
- Remimazolam is sold as a powder and must be reconstituted into a liquid before it can be injected intravenously.
Remimazolam is currently approved as an anesthesia drug in Japan and South Korea, for intensive care unit sedation in Belgium, but only for procedural sedation in the United States, China, and Europe. In total, there are four possible applications for remimazolam. Let’s examine the pros and cons of using remimazolam in these four applications:
- Preoperative sedation. Since midazolam (Versed) was approved in 1982, a standard anesthesia practice has included a 2 mg dose of Versed prior to surgery to calm a patient’s anxiety. In the 1980s my anesthesia chairman at Stanford received a letter from a postoperative patient in which she complained of being awake and very anxious in the operating room prior to the anesthetic for her breast cancer surgery. Our chairman lectured to us, “Do you know many patients are nervous prior to their anesthesia and surgery? Every one of them. We have an excellent drug for relieving preoperative anxiety, and that drug is Versed. Use it! Give your patient a dose of Versed before they enter the operating room. There are few significant side effects of one dose of Versed. Use it!” Will remimazolam replace Versed for this application? No. There is no advantage of the new, shorter acting, more expensive remimazolam over Versed for preoperative sedation.
- Sedation for short procedures. This is the FDA-approved application for remimazolam in the United States. An example procedure would be a colonoscopy. Will remimazolam be widely used for colonoscopies in the near future? No, I doubt it. The cost increase is the main disadvantage. See the typical drug acquisition costs for three alternative sedation recipes for colonoscopy below:
$18.40 for 400 mg of propofol; or
$5.17 for fentanyl+Versed ($4.35 dollars for 6 mg of Versed plus $0.82 for 200 micrograms of fentanyl); or
$41.67 for 20 mg of remimazolam.
The increased cost per case is $23.27 for remimazolam over propofol.
The increased cost per case is $36.50 for remimazolam over fentanyl+Versed.
If a busy endoscopy center does 100 colonoscopies cases per week, the cost increase is $2327 per week for remimazolam over propofol, or $3650 per week for remimazolam over fentanyl+Versed. These are a prohibitive cost increases with no clear added benefits. The only way remimazolam could result in cheaper sedation costs would be if a healthcare system was looking to eliminating the cost of paying for an anesthesia provider for these procedures. The pairing of remimazolam+gastroenterologist sedation rather than propofol+anesthesiologist sedation could afford significant cost savings for a healthcare system.
3. Total intravenous anesthesia (TIVA). TIVA could include a continuous infusion of the ultra-short-acting narcotic remifentanil plus a continuous infusion of the ultra-short-acting remimazolam. An alleged advantage of this technique could be the fast offset time of these two TIVA anesthetic agents. I doubt this technique will gain market share. It’s far easier to turn on the knob of a sevoflurane vaporizer than to load and manage two TIVA-syringe pumps. As well, the added expense of a prolonged infusion of remimazolam will be prohibitive.
4. ICU sedation. Remimazolam has the advantage of ongoing first-degree elimination, meaning that no matter how long the drug is infused, it will always have reliable elimination by esterase and will not accumulate in the plasma. Prolonged ICU sedation with propofol can lead to the Propofol Infusion Syndrome (PRIS). PRIS occurs predominantly in patients receiving high doses of propofol for a prolonged period. Risk factors for the development of PRIS include a critical illness such as sepsis, head trauma, use of vasopressors, and carbohydrate depletion (liver disease, starvation, or malnutrition). PRIS commonly presents as a high anion gap metabolic acidosis, with rhabdomyolysis, hyperkalemia, acute kidney injury, elevated liver enzymes, and decreased cardiac output. Because of the risk of PRIS, the duration of propofol infusion administration should not exceed 48 hours and the administered dose should not be higher than 4 mg/kg/hour.
This potential advantage of remimazolam over propofol will be offset by the increased expense of hours or days of remimazolam utilization in an ICU sedation situation. ICU sedation with fentanyl and older benzodiazepines such as Ativan will have the advantage of a lower cost.
In the hands of an anesthesiologist, propofol is an elegant and almost ideal intravenous sedative, with the advantages of rapid onset, rapid offset, inexpensive generic pricing, minimal cardiovascular/respiratory depression, and lack of nausea. Propofol administration does carry the risks of upper airway obstruction, hypoventilation, and low oxygen saturation, but when an anesthesiologist is present these risks are minimal.
If a healthcare organization doesn’t want to employ an anesthesiologist or a CRNA for a case which requires procedural sedation, then remimazolam may be an excellent sedative choice. Will gastroenterologists prefer to sedate patients with remimazolam plus fentanyl without an anesthesiologist? Or will they prefer to have an anesthesiologist present to administer propofol? Expect gastroenterologists to prefer the latter, because they are not only off-loading the task of sedating the patient, they are also off-loading the risks of managing the patient’s medical co-morbidities, which can be significant if a patient has lung disease, cardiac disease, morbid obesity, or obstructive sleep apnea.
The remimazolam story suggests one of my favorite anecdotes: A former Stanford Chairman of Anesthesiology and friend of mine who left the university in 2006 to become a pharmaceutical company executive, first at Novartis and then at AstraZeneca. Ten years ago, when I asked him what new anesthesia drugs were in the pipeline, he answered, “None, and there probably will be very few new ones. The drugs you have now are inexpensive generic drugs, and they work very well. The research and development costs to bring a new anesthetic drug to market are prohibitively expensive, and unless that new drug is markedly better, it will not push the inexpensive generic drugs out of use.”
Remimazolam will capture a very small market in the United States. Until remimazolam becomes an inexpensive generic drug, I see it as a medical white elephant rather than a wonderful anesthetic advance.

*
*
The most popular posts for laypeople on The Anesthesia Consultant include:
How Long Will It Take To Wake Up From General Anesthesia?
Why Did Take Me So Long To Wake From General Anesthesia?
Will I Have a Breathing Tube During Anesthesia?
What Are the Common Anesthesia Medications?
How Safe is Anesthesia in the 21st Century?
Will I Be Nauseated After General Anesthesia?
What Are the Anesthesia Risks For Children?
The most popular posts for anesthesia professionals on The Anesthesia Consultant include:
10 Trends for the Future of Anesthesia
Should You Cancel Anesthesia for a Potassium Level of 3.6?
12 Important Things to Know as You Near the End of Your Anesthesia Training
Should You Cancel Surgery For a Blood Pressure = 170/99?
Advice For Passing the Anesthesia Oral Board Exams
What Personal Characteristics are Necessary to Become a Successful Anesthesiologist?
READ ABOUT RICK NOVAK’S FICTION WRITING AT RICK NOVAK.COM.

