emailrjnov@yahoo.com
- BRAIN TRANSPLANTATION? - 28 Mar 2024
- THE ANESTHESIA CONSULTANT NAMED THE #1 ANESTHESIOLOGY BLOG IN THE WORLD FOR 2024 BY FEEDSPOT - 7 Mar 2024
- AN ANESTHESIA STORY LIKE NO OTHER - 2 Mar 2024
Recognizing frailty in anesthesia patients is critical.

What if your patients, especially elderly patients, could enter their personal data and symptoms into an iPad app, and what if that information could help you determine if their risk for anesthesia was too great to risk having surgery? Can you imagine this? It will happen someday soon.
Webster’s Dictionary defines frailty as “the condition of being weak and delicate.”
Frailty is also a medical term with an accepted definition of “a multisystem loss of physiologic reserve that makes a person more vulnerable to disability during and after stress.”1

The majority of frail patients are elderly. My training was in both internal medicine and anesthesiology, and the intersection of these two fields is geriatric anesthesia. I have both an interest and expertise in the evaluation and management of geriatric surgery patients. Metrics of frailty exist, and the evaluation of a patient’s frailty index will become an important part of geriatric anesthesia care.
The geriatric population is increasing in size, and the number of elderly patients undergoing surgery is increasing as well. More than half of all operations in the United States are performed on patients of ages ≥65 years, and this proportion will continue to increase.2
In the past a physician’s assessment of a patient’s frailty was an “eyeball” judgment, dependent on how robust versus how frail a patient looked, and dependent on an interpretation of the patient’s active medical problems. Medical researchers began to seek a quantitative metric for frailty, and they proposed frailty evaluation tools.
Dr. Linda Fried developed one of the first frailty indexes in 2001. She studied 5317 men and women 65 years of age or older, and tabulated their answers to questions regarding these five criteria of the Fried Frailty Index: 1,3
- Unintentional weight loss. The patient is asked the question, “In the last year, have you lost more than 10 lb unintentionally (i.e., not as a result of dieting or exercise)?” Patients answering “Yes” are categorized as frail by the weight loss criterion.
- The patient is read the following two statements: (1) I felt that everything I did was an effort; (2) I could not get going. The question is asked, “How often in the last week did you feel this way?” The patient’s response is rated as follows: 0 = rarely or none of the time (<1 day); 1 = some or little of the time (1 to 2 days); 2 = a moderate amount of the time (3 to 4 days); or 3 = most of the time.
- Muscle weakness. The patient is asked about weekly physical activity. Patients with low physical activity are categorized as frail by the physical activity criterion.
- Slowness while walking. The patient is asked to walk a short distance and timed. Patients who are slow walkers are categorized as frail by the walk time criterion.
- Grip strength. The patient’s grip strength is measured. Patients with decreased grip strength are categorized as frail by the grip strength criterion.
Frailty was defined as a clinical syndrome in which three or more of these five criteria were present. The overall prevalence of frailty in this age>65 patient population was 6.9%. The prevalence of frailty increased with age, and was higher in women than men. The frailty phenotype was predictive of falls, worsening mobility or disability, hospitalization, and death. Fried’s conclusion, a novel one at the time, was that “frailty was not synonymous with either comorbidity or disability, but that comorbidity was an etiologic risk factor for frailty, and disability was an outcome of frailty.”
Multiple frailty indexes have been proposed. Velanovich et al proposed a modified Frailty Index using 11 pre-operative variables:4
- History of diabetes
- Impaired functional status
- History of chronic obstructive pulmonary disease or pneumonia
- History of congestive heart failure
- History of MI within 6 months
- History of percutaneous coronary intervention
- Cardiac surgery or angina
- Antihypertensive medication use
- Peripheral vascular disease or rest pain
- Impaired sensory faculties
- History of transient ischemic attack or cerebrovascular accident with persistent residual deficit
This modified Frailty Index correlated positively with the 30-day morbidity and mortality among almost a million patients who underwent surgery between 2005 and 2009 across all surgical specialties.
Other researchers, using a variety of frailty scales, have found that increasing frailty correlates with poorer outcomes after surgery. Researchers at the Seoul National University Bundang Hospital enrolled 275 consecutive elderly patients (aged ≥65 years) who were undergoing intermediate-risk or high-risk elective operations.5
A comprehensive geriatric assessment (CGA) was performed before surgery. The CGA included 6 areas: burden of comorbidity, polypharmacy, physical function, psychological status, nutrition, and risk of postoperative delirium. 9.1% of the patients died during the follow-up period of 11.5-16.1 months, including 4 in-hospital deaths after surgery. 10.5% of the patients experienced at least one complication (e.g., pneumonia, delirium, or urinary tract infection) after surgery, and 8.7% required discharge to inpatient nursing facilities. This CGA frailty score predicted all-cause mortality rates more accurately than the American Society of Anesthesiologists classification. The following factors were associated with increased mortality rates: burden of comorbidity, dependence in activities of daily living, dependence in instrumental activities of daily living, dementia, risk of delirium, short midarm circumference, and malnutrition.
Why was the frailty score more predictive than the ASA score? Geriatric patients often have multiple comorbidities and physiological changes that impair their functional reserve. The assessment of frailty is used to account for these factors.
Contrast the frailty indexes described above to the American Society of Anesthesiologists preoperative assessment scores of ASA 1, 2, 3, 4 , and 5, below:6
| ASA I | A normal healthy patient | Healthy, non-smoking, no or minimal alcohol use |
| ASA II | A patient with mild systemic disease | Mild diseases only without substantive functional limitations. Examples include (but not limited to): current smoker, social alcohol drinker, pregnancy, obesity (30 < BMI < 40), well-controlled DM/HTN, mild lung disease |
| ASA III | A patient with severe systemic disease | Substantive functional limitations; One or more moderate to severe diseases. Examples include (but not limited to): poorly controlled DM or HTN, COPD, morbid obesity (BMI ≥40), active hepatitis, alcohol dependence or abuse, implanted pacemaker, moderate reduction of ejection fraction, ESRD undergoing regularly scheduled dialysis, premature infant PCA < 60 weeks, history (>3 months) of MI, CVA, TIA, or CAD/stents. |
| ASA IV | A patient with severe systemic disease that is a constant threat to life | Examples include (but not limited to): recent ( < 3 months) MI, CVA, TIA, or CAD/stents, ongoing cardiac ischemia or severe valve dysfunction, severe reduction of ejection fraction, sepsis, DIC, ARD or ESRD not undergoing regularly scheduled dialysis |
| ASA V | A moribund patient who is not expected to survive without the operation | Examples include (but not limited to): ruptured abdominal/thoracic aneurysm, massive trauma, intracranial bleed with mass effect, ischemic bowel in the face of significant cardiac pathology or multiple organ/system dysfunction
|
ASA scores are the currently accepted way physicians stratify patient surgical risk. An ASA IV patient with a severe systemic disease that is a constant threat to life will likely have a high frailty index, but the correlation is not absolute. A chronically ill, weak, elderly patient who is losing weight and is inactive may not have an obvious severe systemic disease such as coronary artery disease, cerebral vascular disease, end-stage renal disease, or sepsis, which would qualify them as ASA IV. But a chronically ill, weak, elderly patient who is losing weight and is inactive may have a very high frailty index, and may have a perioperative risk equivalent to any ASA IV patient.
Kennedy created a 30-item Frailty Index in the Canadian Multicentre Osteoporosis Study.7 Their frailty index proved to be a sensitive measure to quantify fracture risk over the next 10 years. McMaster University professors then authored the Fit-Frailty App (available at Apple or Google App Store), a smartphone/iPad app based on the 30-item Canadian Multicentre Osteoporosis Study Frailty Index from the Kennedy study. It takes only minutes for a patient to answer the questions on the app, and the app generates a frailty score, which ranges from 0 to 1.0.
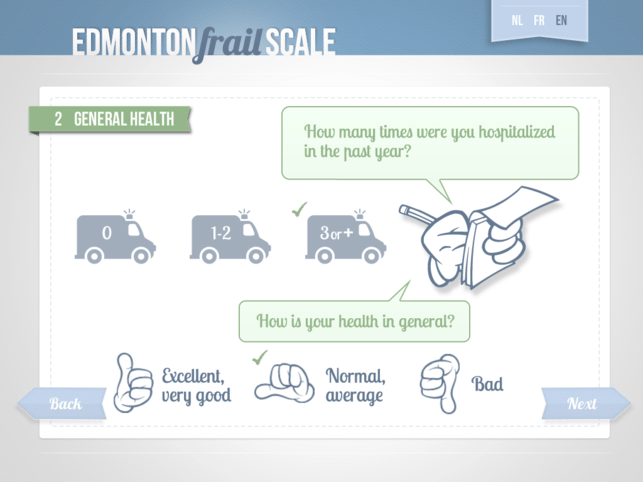
The Edmonton Frail Scale (available at Apple or Google App Store) is a 9-criteria survey which quantifies a frailty score from 0–17. It’s easy to use, and takes about 2–3 minutes to complete.
I predict you’ll see patients filling out frailty apps such as these on iPads in the future, with anesthesiologists and internal medicine doctors using the frailty score as part of their preanesthetic evaluation. You can also expect research on whether intervention or modification of frailty criteria prior to surgery results in lower postoperative complication rates. Frailty index research may lead us to stratify surgical treatments for healthier subsets of geriatric patient populations who are at a lower risk of complications, and provide guidance regarding the proper management of the more frail geriatric patients found to have a higher risk of adverse outcomes after surgery.
Fire up your iPads, download these frailty apps, and see how fit or frail your patients are right now.
References:
- Sieber F, Pauldine R, Geriatric Anesthesia, Miller’s Anesthesia, Chapter 80, 5th edition, 2407-2422.
- Etzioni DA, et al. The aging population and its impact on the surgery workforce. Ann Surg. 2003;238(2):170-177.
- Fried LP et al. Frailty in Older Adults: Evidence for a Phenotype, The Journals of Gerontology: Series A, Volume 56, Issue 3, 1 March 2001, Pages M146–M157.
- Velanovich V, Antoine H, Swartz A, Peters D, Rubinfeld I. Accumulating deficits model of frailty and postoperative mortality and morbidity: its application to a national database. Journal of Surgical Research2013; 183: 104–10.
- Kim S-W et al, Multidimensional Frailty Score for the Prediction of Postoperative Mortality Risk, JAMA Surg. 2014;149(7):633-640.
- https://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system
- Kennedy CC et al, A Frailty Index predicts 10-year fracture risk in adults age 25 years and older: results from the Canadian Multicentre Osteoporosis Study (CaMos) Osteoporosis International, December 2014, Volume 25, Issue 12, pp 2825-2832.
The most popular posts for laypeople on The Anesthesia Consultant include:
How Long Will It Take To Wake Up From General Anesthesia?
Why Did Take Me So Long To Wake From General Anesthesia?
Will I Have a Breathing Tube During Anesthesia?
What Are the Common Anesthesia Medications?
How Safe is Anesthesia in the 21st Century?
Will I Be Nauseated After General Anesthesia?
What Are the Anesthesia Risks For Children?
The most popular posts for anesthesia professionals on The Anesthesia Consultant include:
10 Trends for the Future of Anesthesia
Should You Cancel Anesthesia for a Potassium Level of 3.6?
12 Important Things to Know as You Near the End of Your Anesthesia Training
Should You Cancel Surgery For a Blood Pressure = 178/108?
Advice For Passing the Anesthesia Oral Board Exams
What Personal Characteristics are Necessary to Become a Successful Anesthesiologist?
*
*
*
*
Published in September 2017: The second edition of THE DOCTOR AND MR. DYLAN, Dr. Novak’s debut novel, a medical-legal mystery which blends the science and practice of anesthesiology with unforgettable characters, a page-turning plot, and the legacy of Nobel Prize winner Bob Dylan.
KIRKUS REVIEW
In this debut thriller, tragedies strike an anesthesiologist as he tries to start a new life with his son.
Dr. Nico Antone, an anesthesiologist at Stanford University, is married to Alexandra, a high-powered real estate agent obsessed with money. Their son, Johnny, an 11th-grader with immense potential, struggles to get the grades he’ll need to attend an Ivy League college. After a screaming match with Alexandra, Nico moves himself and Johnny from Palo Alto, California, to his frozen childhood home of Hibbing, Minnesota. The move should help Johnny improve his grades and thus seem more attractive to universities, but Nico loves the freedom from his wife, too. Hibbing also happens to be the hometown of music icon Bob Dylan. Joining the hospital staff, Nico runs afoul of a grouchy nurse anesthetist calling himself Bobby Dylan, who plays Dylan songs twice a week in a bar called Heaven’s Door. As Nico and Johnny settle in, their lives turn around; they even start dating the gorgeous mother/daughter pair of Lena and Echo Johnson. However, when Johnny accidentally impregnates Echo, the lives of the Hibbing transplants start to implode. In true page-turner fashion, first-time novelist Novak gets started by killing soulless Alexandra, which accelerates the downfall of his underdog protagonist now accused of murder. Dialogue is pitch-perfect, and the insults hurled between Nico and his wife are as hilarious as they are hurtful: “Are you my husband, Nico? Or my dependent?” The author’s medical expertise proves central to the plot, and there are a few grisly moments, as when “dark blood percolated” from a patient’s nostrils “like coffee grounds.” Bob Dylan details add quirkiness to what might otherwise be a chilly revenge tale; we’re told, for instance, that Dylan taught “every singer with a less-than-perfect voice…how to sneer and twist off syllables.” Courtroom scenes toward the end crackle with energy, though one scene involving a snowmobile ties up a certain plot thread too neatly. By the end, Nico has rolled with a great many punches.
Nuanced characterization and crafty details help this debut soar.
Click on the image below to reach the Amazon link to The Doctor and Mr. Dylan:
LEARN MORE ABOUT RICK NOVAK’S FICTION WRITING AT RICK NOVAK.COM BY CLICKING ON THE PICTURE BELOW:



